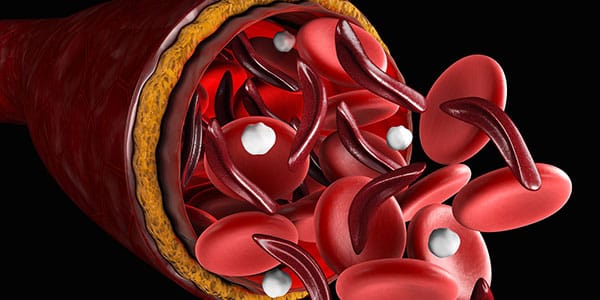
Despite “matching,” harmful RBC alloantibodies sickle cell disease patients still happen. Are we doing enough?
NOTE: Continuing Education credit for this episode has expired. See below for details.

Dr. Stella Chou
A Pediatric Hematologist Weighs In
Dr. Stella Chou, an expert pediatric hematologist, has spent most of her career improving methods to match red cells in patients with SCD. She noted early on that some of her patients who she didn’t think should make Rh antibodies did so! For example, she saw E-negative patients with SCD form anti-E antibodies even though they had received blood from donors who were also E-negative. This happened despite her patients receiving blood from “matched” African-American blood donors. Most importantly, in many cases, these antibodies led to delayed hemolytic transfusion reactions. This is a big problem, and we should all wonder, “Are we doing enough?”
Preventing Alloantibodies in Sickle Cell Patients
Stella and her co-authors (including Connie Westhoff, who has spoken about Rh genotyping on this podcast in the past), reported these surprising finding in 2013 (reference below). In this interview, she discusses how incredibly common variant RH alleles are in patients with SCD and minority blood donors, and how those variants contribute to Rh alloimmunization. She also describes innovative strategies that may hold the key to reducing alloimmunization using RH genetic matching of donors and patients in the future.

Dr. Stella Chou
A Pediatric Hematologist Weighs In
Dr. Stella Chou, an expert pediatric hematologist, has spent most of her career improving methods to match red cells in patients with SCD. She noted early on that some of her patients who she didn’t think should make Rh antibodies did so! For example, she saw E-negative patients with SCD form anti-E antibodies even though they had received blood from donors who were also E-negative. This happened despite her patients receiving blood from “matched” African-American blood donors. Most importantly, in many cases, these antibodies led to delayed hemolytic transfusion reactions. This is a big problem, and we should all wonder, “Are we doing enough?”
Preventing Alloantibodies in Sickle Cell Patients
Stella and her co-authors (including Connie Westhoff, who has spoken about Rh genotyping on this podcast in the past), reported these surprising finding in 2013 (reference below). In this interview, she discusses how incredibly common variant RH alleles are in patients with SCD and minority blood donors, and how those variants contribute to Rh alloimmunization. She also describes innovative strategies that may hold the key to reducing alloimmunization using RH genetic matching of donors and patients in the future.
About My Guest:
Dr. Stella Chou is an Associate Professor of Pediatrics at the Perelman School of Medicine at the University of Pennsylvania. She practices Pediatric Hematology and Transfusion Medicine at The Children’s Hospital of Philadelphia with a particular interest in patients with Sickle Cell Disease. Her work has demonstrated that inheritance of variant blood group antigens in patients with Sickle Cell Disease contributes to their high rate of red cell antibody formation.
Dr. Chou’s research interests include improving red blood cell matching for patients using innovative tools. Her research laboratory uses induced pluripotent stem cells (iPSCs) and primary human cells to model blood diseases and study their underlying pathophysiology. Her ongoing work focuses on creating customized iPSCs with rare blood group antigen combinations as renewable sources of red cell reagents to improve antibody identification and donor red cell matching. Since transfusion therapy remains a critical treatment for hemoglobinopathies, her goal is to identify new approaches to minimize alloimmunization, reduce complications and improve therapy.
Continuing Education Expired
This podcast episode offered continuing education credit for two years from its release date, but is no longer eligible for such credit.
To find Blood Bank Guy Essentials Podcast episodes with active continuing education opportunities, Click here or visit Transfusion News Continuing Education on Wiley Health Learning.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Dr. Chou nor I have any relevant financial disclosures.
Further Reading:
- 2013 study showing shockingly high rates of antibodies in patients with sickle cell disease transfused with matched RBCs from minority blood donors: Chou ST et al. High prevalence of red blood cell alloimmunization in sickle cell disease despite transfusion from Rh-matched minority donors. Blood 2013;122(6):1062-1071.
- 2018 study reporting on rates of RH variants in African-American blood donors AND feasibility of a genotype-matched donor pool: Chou ST et al. RH genotype matching for transfusion support in sickle cell disease. Blood 2018;132(11):1198-1207.
- 2019 study detailing the underrecognition of delayed hemolytic reactions in patients with sickle cell disease after alloimmunization: Coleman S et al. Alloimmunization in patients with sickle cell disease and underrecognition of accompanying delayed hemolytic transfusion reactions. Transfusion 2019 (early view).
Thanks to:
- Dr. Daniela Hermelin, Assistant Editor; Please follow Daniela on Twitter for fantastic #blooducation!
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














I would like to suggest two other possible contributing factors to the high alloimmunization and auto-antibody rate in sickle cells patients, and to the high incidence of increased hemolysis reported.
Firstly, use of unwashed group O red cells (particularly for red cell exchange) in non-O patients may contribute to both alloimmunization and hemolysis. While the volume of plasma containing anti-A and Anti-B is small, repeated use of group O red cells undoubtedly contributes to low level (sub-clinical) hemolysis in these patients. Most blood centers provide antigen screened group O red cells for these patients and this is sub-optimal for group A, B and AB patients.
It is not widely appreciated, but ABO immune complexes contribute to hemolysis in patients. In vitro, this is absolutely clear, and it seems likely the same would occur in vivo.
Vox Sang. 2016 Apr;110(3):219-26. doi: 10.1111/vox.12354. Epub 2015 Nov 3.
ABO-immune complex formation and impact on platelet function, red cell structural integrity and haemostasis: an in vitro model of ABO non-identical transfusion.
Zaffuto BJ1,2, Conley GW3, Connolly GC1,2, Henrichs KF3, Francis CW1,2, Heal JM1,2, Blumberg N3, Refaai MA3.
Author information
Abstract
BACKGROUND:
Transfusion of ABO non-identical platelets has been associated with fatal haemolytic reactions, increased red cell transfusion needs and other adverse effects, but the practice of ABO matching in platelet transfusion is controversial. Immune complexes can be formed from the anti-A and/or anti-B antibodies and ABO soluble antigen(s) present in donor and recipient plasma after ABO non-identical transfusions. We hypothesized that these immune complexes affect recipient red cell structural integrity, platelet function and haemostasis.
STUDY DESIGN AND METHODS:
Haemolysis, platelet function and haemostatic function were assessed before and after incubation of recipient red cells, platelets and whole blood with normal saline controls, ABO-identical plasma controls or in vitro-generated ABO-immune complexes.
RESULTS:
ABO-immune complexes caused significantly increased haemolysis (P < 0·001), inhibition of platelet function (P = 0·001) and disruption of clot formation kinetics (P < 0·005) in both group A and O recipient samples.
CONCLUSIONS:
Substantial changes in platelet function, red cell integrity and haemostasis occur after in vitro exposure to immune complexes. These in vitro findings may explain, in part, previously observed associations of ABO non-identical platelet transfusions with adverse effects including increased red cell transfusion needs, organ failure and mortality.
Secondly, ABO non-identical transfusions contribute significantly to alloimmunization to non-ABO antigens, including HLA and platelet specific antibodies. (Carr, Br. J. Haem, 1990, see below).
When we stopped infusing ABO mismatched antibody and soluble/cellular antigen, rbc alloimmunization rates dropped gradually by 50% in our center in all patients.
Transfusion. 2012 Mar;52(3):635-40. doi: 10.1111/j.1537-2995.2011.03329.x. Epub 2011 Sep 2.
Providing ABO-identical platelets and cryoprecipitate to (almost) all patients: approach, logistics, and associated decreases in transfusion reaction and red blood cell alloimmunization incidence.
Henrichs KF1, Howk N, Masel DS, Thayer M, Refaai MA, Kirkley SA, Heal JM, Blumberg N.
Author information
Abstract
BACKGROUND:
There are multiple benefits to transfusing only ABO-identical blood components. Historically our institution routinely transfused ABO-nonidentical platelets (PLTs) and cryoprecipitate to surgical patients. In April 2005, we implemented a policy of transfusing only ABO-identical components whenever feasible, regardless of outdating or logistic considerations.
STUDY DESIGN AND METHODS:
Technical staff closely monitored product usage and adjusted blood center orders based on recent utilization and planned transfusions. When unable to provide ABO-identical PLTs, ABO-compatible PLTs were washed to remove incompatible plasma. Data on outdating were collected for 18 months before and after implementation. We compared transfusion reaction and red blood cell (RBC) alloimmunization incidence for 4 years preceding (2001-2004) and subsequent (2006-2009) to implementation.
RESULTS:
In the year after implementation, only 11 of 410 surgical patients received ABO-nonidentical PLTs (2.7%). There was a 5.6% increase in outdating of PLTs. Transfusing ABO-identical components was associated with significant reductions in febrile (-46%; 8.0 to 4.3 per 10,000 components; p < 0.0001) and allergic transfusion reactions (-23%; from 7.0 to 5.4 per 10,000 components; p = 0.025). A progressive reduction in de novo RBC alloimmunization incidence also occurred (-50% by 2009; p = 0.03).
CONCLUSIONS:
Providing ABO-identical PLTs to almost all patients was feasible in our setting by changing ordering and inventorying procedures and making the ABO-identical policy a staff priority. Unexpected and striking reductions in febrile and allergic reactions and RBC alloimmunization were observed, of uncertain causal relationship to this ABO policy change, which will require further study.
Br J Haematol. 1990 Jul;75(3):408-13.
Transfusion of ABO-mismatched platelets leads to early platelet refractoriness.
Carr R1, Hutton JL, Jenkins JA, Lucas GF, Amphlett NW.
Author information
Abstract
Forty-three consecutive patients previously unexposed to platelets and undergoing treatment for acute leukaemia or autografting for relapsed Hodgkin's lymphoma were randomized to receive transfused platelets of either their own ABO group (OG) or of a major mismatched group (MMG). The 26 evaluable patients were equally distributed between the two study groups. Nine of 13 (69%) MMG patients became refractory with a median onset at transfusion 7 (15 d), compared with only one of 13 (8%) OG patients (P = 0.001). Refractoriness was associated with the formation of high titre isoagglutinins, anti-HLA and platelet specific antibodies. In one patient refractoriness appeared to be due to high titre isoagglutinins alone. Six other patients developed an increase in isoagglutinin titre sufficient to adversely affect platelet increments. Patients receiving ABO-mismatched platelets had a higher incidence of anti-HLA antibodies (5 v. 1) and platelet specific antibodies (4 v. 1). ABO-mismatched platelets transfused prior to the onset of refractoriness resulted in increments similar to those achieved by ABO-matched platelets. The study demonstrates that ABO-mismatched platelets are as effective as matched platelets in patients with low titre isoagglutinins requiring only few transfusions. However, the greater incidence of early refractoriness induced in MMG patients indicates that ABO-mismatched platelets should not be given to patients with marrow failure requiring long-term support.
Hope these clues will provide some utility to those interested in the problem of sub-clinical hemolysis and alloimmunization. Our policies of "univeral ABO" blood group transfusions are almost certainly contributing to both clinical issues.