A 25-year-old, A negative female needs blood. She will receive RhD-negative RBCs, of course, but what about antigen matching for Kell, or for other Rh antigens? Meghan Delaney explains the “AMIGO Study.”

Dr. Meghan Delaney
But What About Transfusion’s Role?
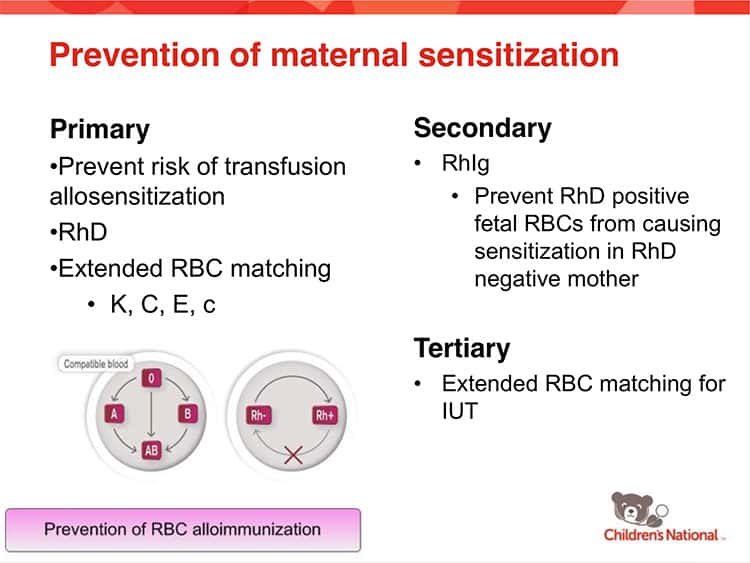
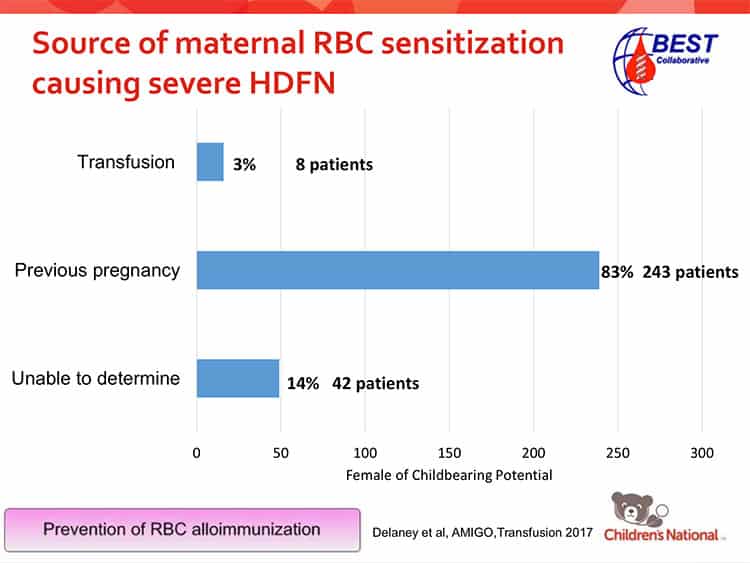
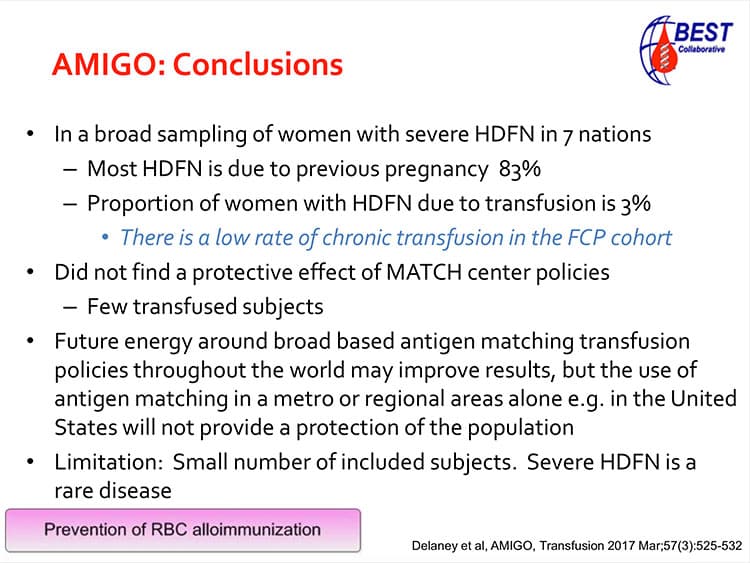
Of course, we’ve also always known that transfusion could be the event that causes mom to make an antibody, instead of pregnancy. What we haven’t really known is how often transfusion causes the problem compared to pregnancy. We also wondered if matching RBC transfusions for antigens like K or c would decrease the risk of severe HDFN. This has led to varying practices and restrictions internationally, with some countries requiring females of child-bearing potential to be matched for additional red cell antigens (beyond the standard matching for RhD). So, females below a certain age in these countries who are K-negative, for example, are given K-negative RBCs when transfused in an effort to reduce transfusion-induced anti-K formation (and some countries go well beyond matching for K). Such matching is not a requirement in the United States.
Along Comes “AMIGO!”
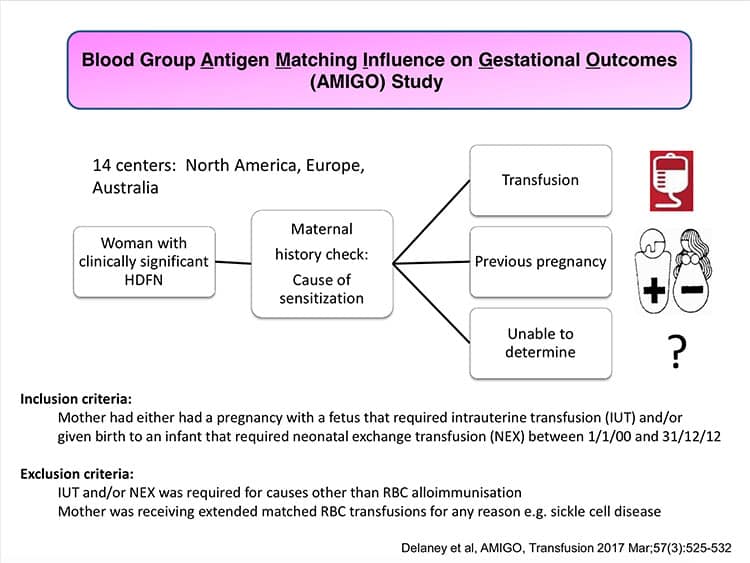
In the “Blood Group Antigen Matching Influence on Gestational Outcomes,” or AMIGO Study, Dr. Meghan Delaney and her BEST Collaborative group decided to look at this issue. They first wanted to see what proportion of moms delivering babies with severe HDFN had transfusion histories vs pregnancy-only histories. Another goal was to try to answer the question of whether or not a prophylactic strategy aimed at decreasing the risk of non-D alloimmunization in females of childbearing potential was effective. Meghan is here today to talk about her role in that study and to tell us what the group was able to find out.

Dr. Meghan Delaney
But What About Transfusion’s Role?
Of course, we’ve also always known that transfusion could be the event that causes mom to make an antibody, instead of pregnancy. What we haven’t really known is how often transfusion causes the problem compared to pregnancy. We also wondered if matching RBC transfusions for antigens like K or c would decrease the risk of severe HDFN. This has led to varying practices and restrictions internationally, with some countries requiring females of child-bearing potential to be matched for additional red cell antigens (beyond the standard matching for RhD). So, females below a certain age in these countries who are K-negative, for example, are given K-negative RBCs when transfused in an effort to reduce transfusion-induced anti-K formation (and some countries go well beyond matching for K). Such matching is not a requirement in the United States.
Along Comes “AMIGO!”
In the “Blood Group Antigen Matching Influence on Gestational Outcomes,” or AMIGO Study, Dr. Meghan Delaney and her BEST Collaborative group decided to look at this issue. They first wanted to see what proportion of moms delivering babies with severe HDFN had transfusion histories vs pregnancy-only histories. Another goal was to try to answer the question of whether or not a prophylactic strategy aimed at decreasing the risk of non-D alloimmunization in females of childbearing potential was effective. Meghan is here today to talk about her role in that study and to tell us what the group was able to find out.

Dr. Meghan Delaney
But What About Transfusion’s Role?
Of course, we’ve also always known that transfusion could be the event that causes mom to make an antibody, instead of pregnancy. What we haven’t really known is how often transfusion causes the problem compared to pregnancy. We also wondered if matching RBC transfusions for antigens like K or c would decrease the risk of severe HDFN. This has led to varying practices and restrictions internationally, with some countries requiring females of child-bearing potential to be matched for additional red cell antigens (beyond the standard matching for RhD). So, females below a certain age in these countries who are K-negative, for example, are given K-negative RBCs when transfused in an effort to reduce transfusion-induced anti-K formation (and some countries go well beyond matching for K). Such matching is not a requirement in the United States.
Along Comes “AMIGO!”
In the “Blood Group Antigen Matching Influence on Gestational Outcomes,” or AMIGO Study, Dr. Meghan Delaney and her BEST Collaborative group decided to look at this issue. They first wanted to see what proportion of moms delivering babies with severe HDFN had transfusion histories vs pregnancy-only histories. Another goal was to try to answer the question of whether or not a prophylactic strategy aimed at decreasing the risk of non-D alloimmunization in females of childbearing potential was effective. Meghan is here today to talk about her role in that study and to tell us what the group was able to find out.

About My Guest:
Meghan Delaney, DO, MPH is Chief of the Department of Pathology & Laboratory Medicine at Children’s National Health System in Washington, DC, as well as Associate Professor in the Departments of Pathology and Pediatrics at the George Washington University School of Medicine in Washington, DC. She arrived in DC in 2017 following a highly distinguished decade of service at Bloodworks Northwest (the former Puget Sound Blood Center) and the University of Washington in Seattle. Dr. Delaney is board-certified in Clinical Pathology as well as in Blood Banking/Transfusion Medicine.
Meghan serves on numerous committees and editorial boards both nationally and internationally (too many to list, trust me!). In addition, she has authored or co-authored over 60 papers in peer-reviewed journals, and 18 book chapters, and over 40 abstracts. She speaks all over the world on a wide variety of topics in adult, pediatric, obstetric, and molecular Transfusion Medicine. Finally, she is an associate editor of the 20th edition of my top-recommended textbook for those learning the essentials of Transfusion Medicine, the AABB Technical Manual.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone. Statements made on this podcast are not official opinions of the organizations with which either of us is affiliated. Neither Meghan nor I have any relevant financial disclosures.
The images below are generously provided by Dr. Meghan Delaney.
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














BRILLIANT (as ever). Just one question, given that the frequency of the expression of the K antigen varies enormously between the various populations, was this taken into account? For example, a woman with anti-K from the White population in the UK, who has a White male partner has (roughly) a 9% chance that this partner would be K+k+, but a woman with anti-K from the Black population in the UK, who has a Black male partner would only have (roughly) a 2% chance that her partner would be K+k+.
Malcolm, I’m grateful for the kind word. I forwarded your question to Dr. Delaney, and here is her response:
Thank you both for your swift and polite answer.
I love it on here!
Given the hospitals are now paid by diagnostic codes instead of by tests, the less we spend on the patients the better for the bottom line. For the past few years, we have a hard time convincing the bb supervisors for additional tests, like getting antigen profile of patients before starting anti-CD38 or 47. They prefer wait and see. When time comes the reference lab can use DTT etc to figure out.
Unless AABB or CAP said all females below age 50 or 55 get K matched prbc, like Dr. Delaney suggested, I am pretty sure my bb supervisors will not say yes to the K testing.
CAP had dinged hospitals for drawing additional tubes that no test was attached to, like ED drawing additional blue or grey tops. Is CAP in the mood to add K testing for females?