Patients with liver disease receive almost 1 of every 5 blood products transfused in hospitals! Dr. Jeannie Callum thinks that is too much, and she shares how we can improve our practice in these complex patients.
NOTE: Continuing Education credit for this episode has expired. See below for details.

Dr. Jeannie Callum
But Wait!
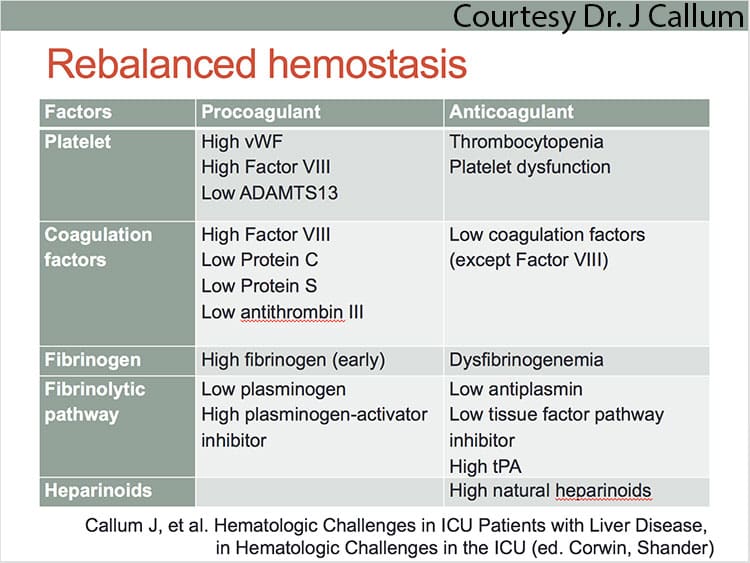
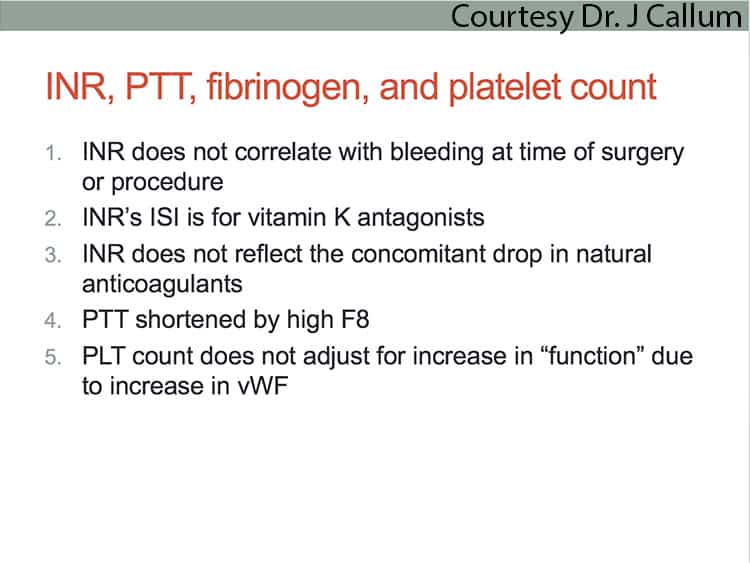
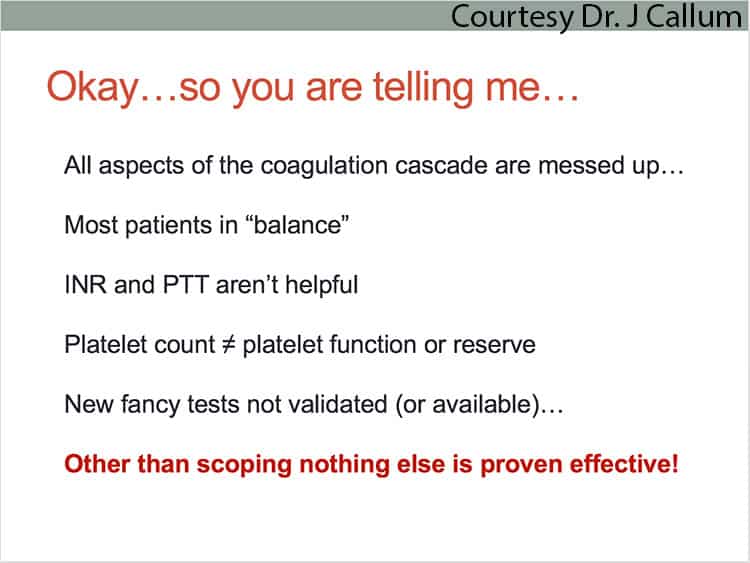
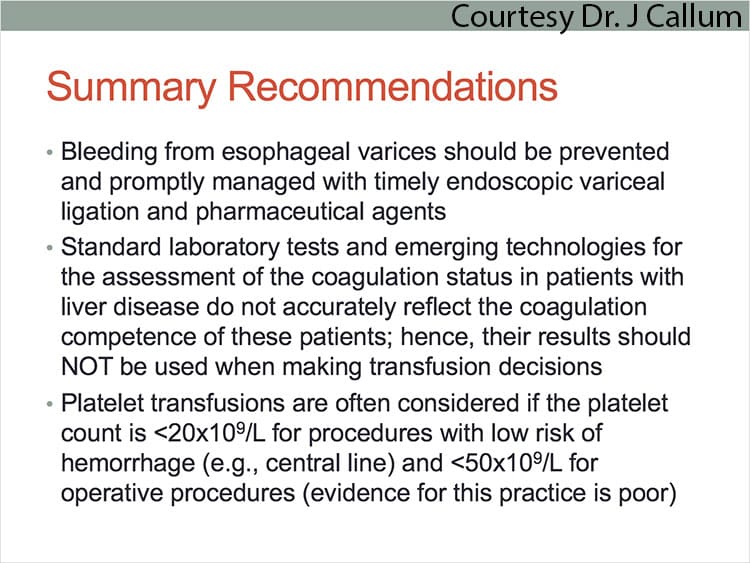
Dr. Jeannie Callum, an outstanding Transfusion Medicine physician who also happens to be a clinician, says that the laboratory picture usually doesn’t tell us the whole story! She explains the complex coagulation disturbance seen in patients with liver disease, and helps us understand that these patients are actually better than their lab tests make them seem (in fact, they may actually be at risk of clotting if we transfuse them!). Jeannie explains the “rebalanced” coagulation system and the reasons why these patients get thrombocytopenic (and why just looking at the platelet count would lead you to be overly pessimistic). She then takes us on a tour of non-transfusion and transfusion choices for patients with liver disease. This interview is guaranteed to open your eyes to things you may not have known!

Dr. Jeannie Callum
But Wait!
Dr. Jeannie Callum, an outstanding Transfusion Medicine physician who also happens to be a clinician, says that the laboratory picture usually doesn’t tell us the whole story! She explains the complex coagulation disturbance seen in patients with liver disease, and helps us understand that these patients are actually better than their lab tests make them seem (in fact, they may actually be at risk of clotting if we transfuse them!). Jeannie explains the “rebalanced” coagulation system and the reasons why these patients get thrombocytopenic (and why just looking at the platelet count would lead you to be overly pessimistic). She then takes us on a tour of non-transfusion and transfusion choices for patients with liver disease. This interview is guaranteed to open your eyes to things you may not have known!
About My Guest:
Jeannie L. Callum, MD, FRCPC, is a Transfusion Medicine Specialist and Hematologist at Sunnybrook Health Sciences Center in Toronto and associate professor of the Department of Laboratory Medicine and Pathobiology at the University of Toronto. She is the Director of Utilization for the Department of Laboratory Medicine and Molecular Diagnostics. She also serves as the sponsor lead for the Ontario Regional Blood Coordinating Network for Central Ontario.
Dr. Callum earned her medical degree and completed a fellowship in internal medicine at the University of Toronto. In addition, she received transfusion medicine fellowship training with Canadian Blood Services. She has written extensively about issues in Transfusion Medicine, publishing more than 100 peer-reviewed articles and authoring numerous book chapters. She also was the lead author on the Provincial (Ontario) transfusion handbook titled “Bloody Easy,” now in its fourth edition (if you don’t have it already, go to transfusionontario.org and get a free download!). In addition, she is on the editorial board for the “Transfusion Medicine Reviews” and “Transfusion” journals.
Continuing Education Expired
This podcast episode offered continuing education credit for two years from its release date, but is no longer eligible for such credit.
To find Blood Bank Guy Essentials Podcast episodes with active continuing education opportunities, Click here or visit Transfusion News Continuing Education on Wiley Health Learning.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. See the Wiley Health Learning site for Dr. Callum’s disclosures. Dr. Chaffin has no relevant financial disclosures.
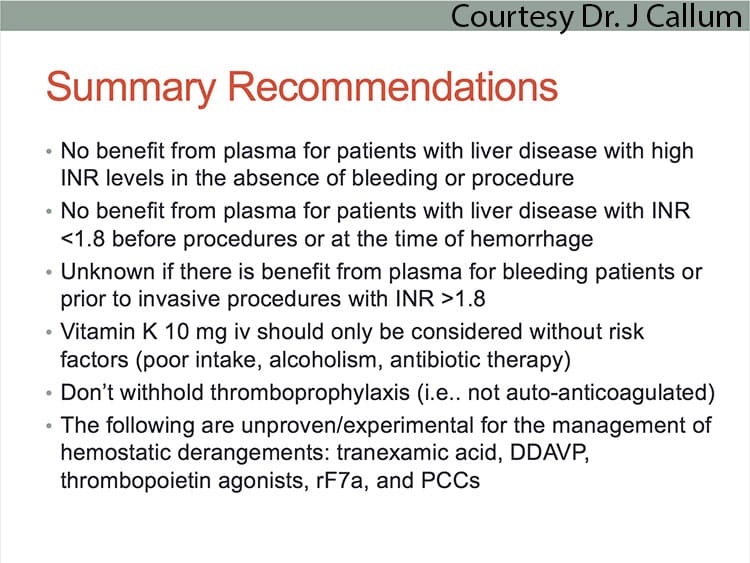
The images below are generously provided by Dr. Callum.
Further Reading:
- Kaufman RM, et al. Platelet Transfusion: A Clinical Practice Guideline From the AABB. Ann Intern Med. 2015;162(3):205-13
- Lisman T et al. Intact thrombin generation and decreased fibrinolytic capacity in patients with acute liver injury or acute liver failure. J Thromb Haem 2012;20:1312-1319
- Desborough MJ et al. Patterns of blood component use in cirrhosis: A nationwide study. Liver Int. 2016;36:522-529
- Jia Q et al. Prophylactic plasma transfusion for surgical patients with abnormal preoperative coagulation tests: A single-institution propensity-adjusted cohort study. Lancet Haematology 2016;3:e139-148
- Warner MA et al. Changes in International Normalized Ratios After Plasma Transfusion of Varying Doses in Unique Clinical Environments. Anesth and Analg 2018;127:349-357
- The HALT_IT Trial evaluating use of tranexemic acid in gastrointestinal bleeding
- Choosing Wisely Canada Transfusion Recommendations (especially note #3)
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














Hi Dr. Chaffin,
Great podcast fill with lots of awesome information. The one question I had is with regards to fibrinogen levels. Dr. Callum mentioned that patients with liver disease often have elevated fibrinogen due to being an acute phase reactant. As the liver is the site of fibrinogen synthesis, wouldn’t patients with liver failure have decreased fibrinogen levels (Lisman, T. et al. https://www.karger.com/Article/FullText/103655)? Moreover, it’s been reported these patients can get a dysfibrinogenemia due to excess sialic acid residues on the fibrinogen.
Although thrombin generation is comparable to controls, if these patients have reduced fibrinogen, they will have difficulty forming a clot. At my institution, we recommend cirrhotic patients who are bleeding or undergoing an invasive procedure, to maintain a fibrinogen level of 150 mg/dl or 100 mg/dl respectively with the use of cryoprecipitate. Do you or Dr. Callum have any thoughts on the use of cryoprecipitate for these patients? The lower volume while providing fibrinogen could be useful for these patients.
Thank you,
Chuck
Chuck, I asked Dr. Callum for her thoughts on your comment, and here is her reply:
“Great question!
We need someone to study this!
Fibrinogen level is either preserved or elevated in patients with liver disease. (1) This is from chronic low grade bacteremia causing inflammatory rise; obviously early in disease where the synthetic function of the liver can still pump it out. To further complicate matters, patients with liver disease produce abnormal and hypofunctional fibrinogen proteins due to increased sialic acid residues leading to impaired polymerization; how much this causes a problem we don’t know – likely later in liver progression. (2) We don’t know when to give cryo. The protocol at my hospital is (1) mild bleeding if <100; (2) serious hemorrhage <200.
1.Stein SF, Harker LA. Kinetic and functional studies of platelets, fibrinogen, and plasminogen in patients with hepatic cirrhosis. J Lab Clin Med. 1982;99(2):217-30.
2.Francis JL, Armstrong DJ. Fibrinogen-bound sialic acid levels in the dysfibrinogenaemia of liver disease. Haemostasis. 1982;11(4):215-22."
Dr. Chaffin:
Another great episode!
I have a somewhat related question. Dr. Callum referenced giving 10 mg of IV vitamin K to reverse warfarin in hospitalized patients.
At my medical center we have an order set that calls for varying doses of either oral or IV vitamin K to reverse warfarin ahead of invasive procedures based on the patient’s INR (higher INR gets higher dose). The Thrombosis Canada app basically recommends 10 mg of IV vitamin K for any INR greater than 1.5.
Is this approach evidenced based? Are there any references?
Thank you!
Bruce, I called your question to Dr. Callum’s attention, and she got REALLY excited! Here’s her response:
This is one of my favorite topics to cover with the medical residents on hematology consults or when we are bored in clinic waiting for a patient.
BASICS YOU MUST MEMORIZE (You will use this knowledge often):
Jeannie notes that most of the evidence for this is in her 2014 commentary to accompany the AABB’s recommendations for the American Board of Internal Medicine “Choosing Wisely” campaign (the commentary is in Transfusion 2014;54:2344-2352).