Red cell antibodies should be simple, right? Not always, and the Mighty Monocyte Monolayer Assay may show the way!
NOTE: Continuing Education credit for this episode has expired. See below for details.

Sandy Nance MS, MASCP, MT(ASCP)SBB
The Mighty MMA Shows The Way!
Back in the 1980’s, blood bankers were using many different tests to try to answer that question, but many of those tests were complex and logistically challenging. Sandy Nance and a group of other illustrious scientists at the American Red Cross developed the monocyte monolayer assay to try to help us with the choice of whether or not a patient with an antibody against a high-frequency antigen can be safely given antigen-positive blood. The MMA is simple in concept, but labor-intensive, so not very many labs do it, and you may or may not have heard of it. After today, I think you will have a much better understanding of what the test is, and how it can really help in some “no-win” situations.

Sandy Nance MS, MASCP, MT(ASCP)SBB
The Mighty MMA Shows The Way!
Back in the 1980’s, blood bankers were using many different tests to try to answer that question, but many of those tests were complex and logistically challenging. Sandy Nance and a group of other illustrious scientists at the American Red Cross developed the monocyte monolayer assay to try to help us with the choice of whether or not a patient with an antibody against a high-frequency antigen can be safely given antigen-positive blood. The MMA is simple in concept, but labor-intensive, so not very many labs do it, and you may or may not have heard of it. After today, I think you will have a much better understanding of what the test is, and how it can really help in some “no-win” situations.
About My Guest:
Sandy Nance is the emeritus Senior Director for National Laboratories for the American Red Cross and has provided leadership to multiple programs at the Red Cross and blood bank world in general, including the American Rare Donor Program and the national American Red Cross SBB Program. She is also an emeritus Adjunct Assistant Professor at the University of Pennsylvania, Division of Transfusion Medicine & Therapeutic Pathology Department of Pathology and Laboratory Medicine. She has a master’s degree in Pathology from the University of Maryland and received her SBB from the Johns Hopkins Medical Institutions. Sandy developed of the use of polyethylene glycol or PEG for serologic testing as well as today’s topic, the monocyte monolayer assay (MMA).
Sandy’s list of honors and awards is too long to detail, but they include the John Elliott, President’s, and Sally Frank awards from AABB, the National Blood Foundation Hall of Fame, the ASCP Hall of Fame. She has authored or co-authored over 45 scientific papers and 200 abstracts, and edited 9 books.
Her career positions include Lead Technologist at Johns Hopkins Medical Institutions with Dr. Paul Ness and Immunohematology Research Associate in Dr. George Garratty’s Research Laboratory. Active in education, she has been faculty for University of Maryland, Johns Hopkins Medical Institutions, University of Pennsylvania, NIH and American Red Cross.
Continuing Education Expired
This podcast episode offered continuing education credit for two years from its release date, but is no longer eligible for such credit.
There are currently no episodes of Blood Bank Guy Essentials eligible for continuing education credit, but check back soon!
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Sandy nor I have any relevant financial disclosures.
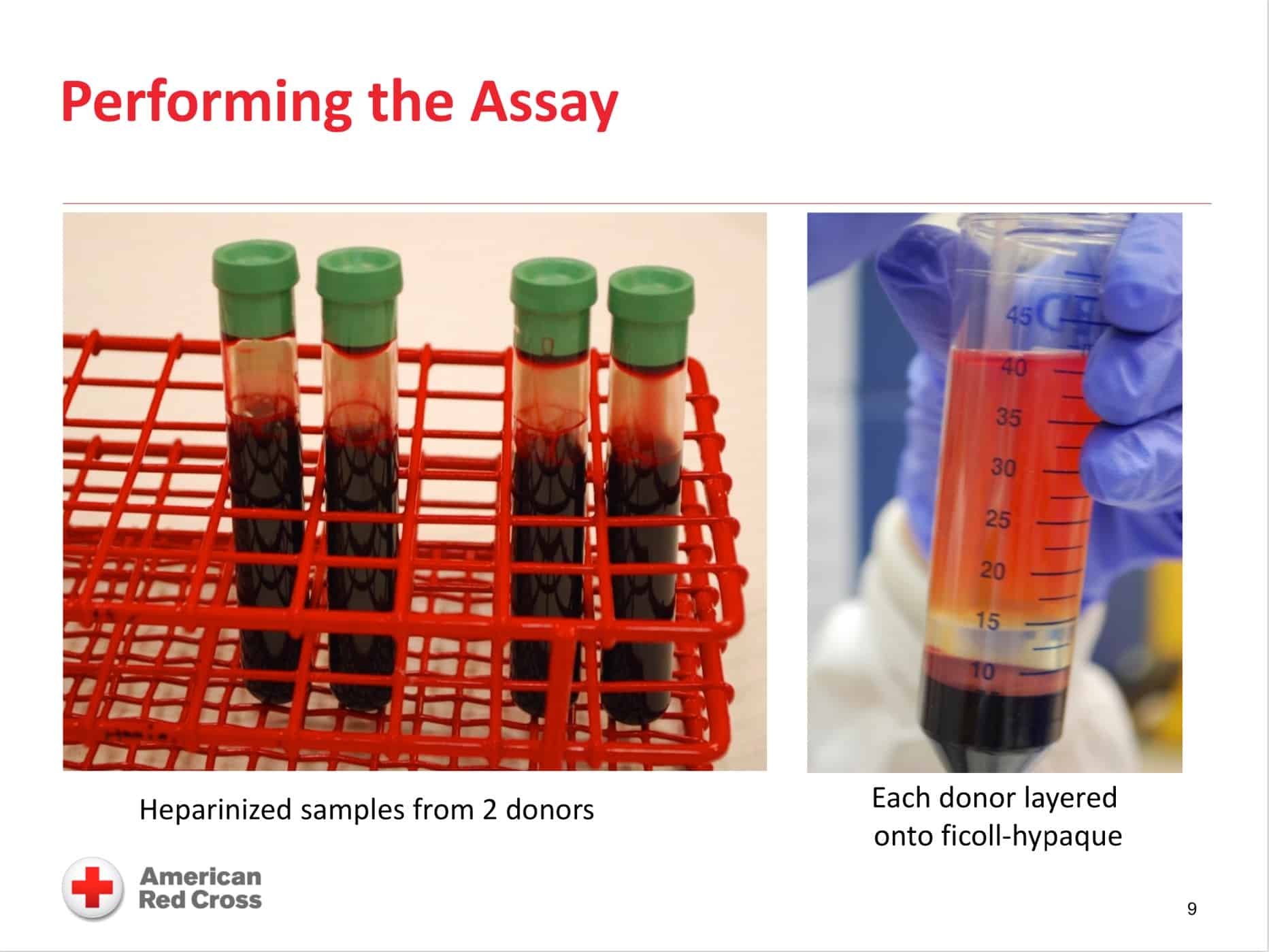
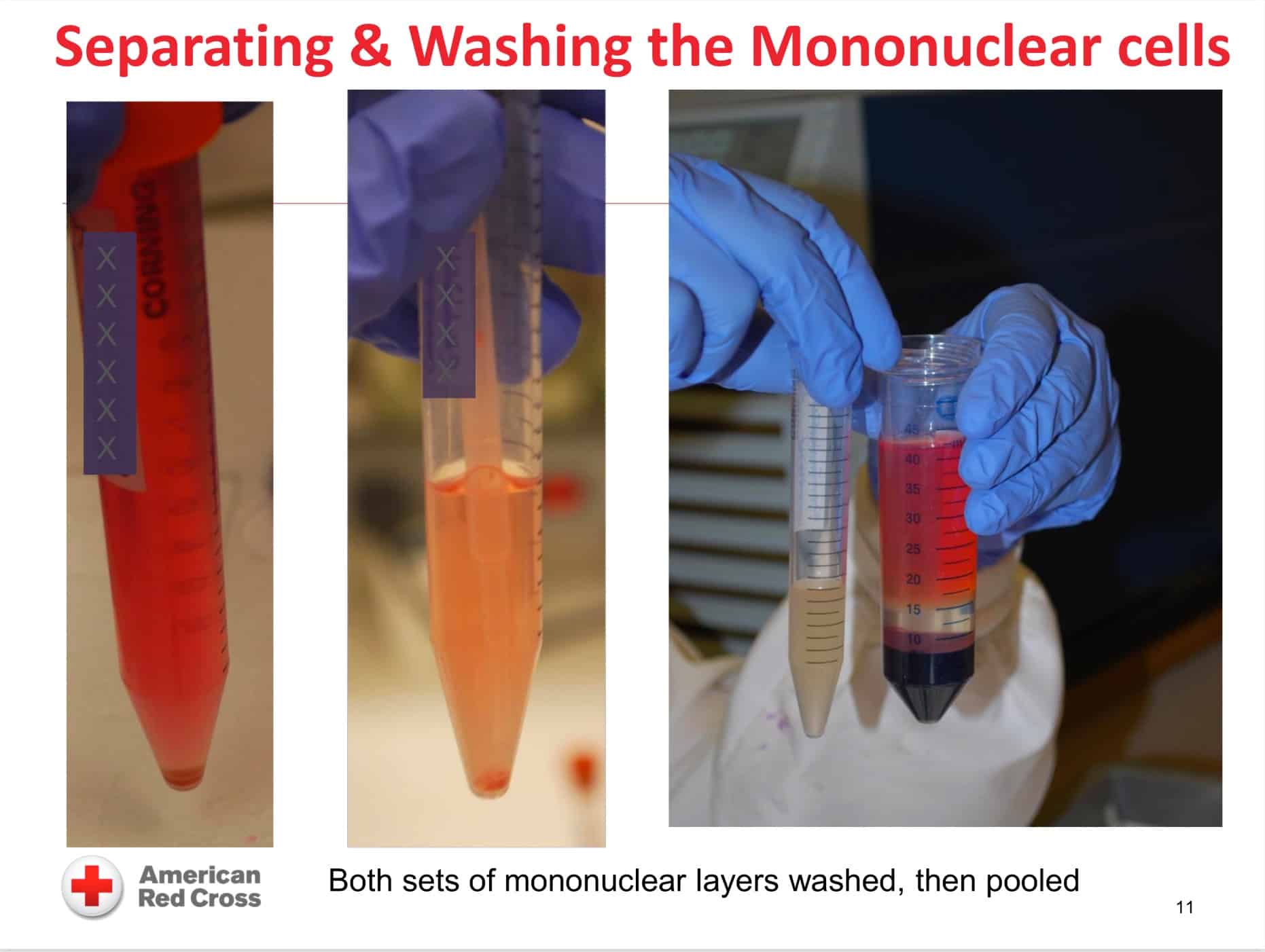
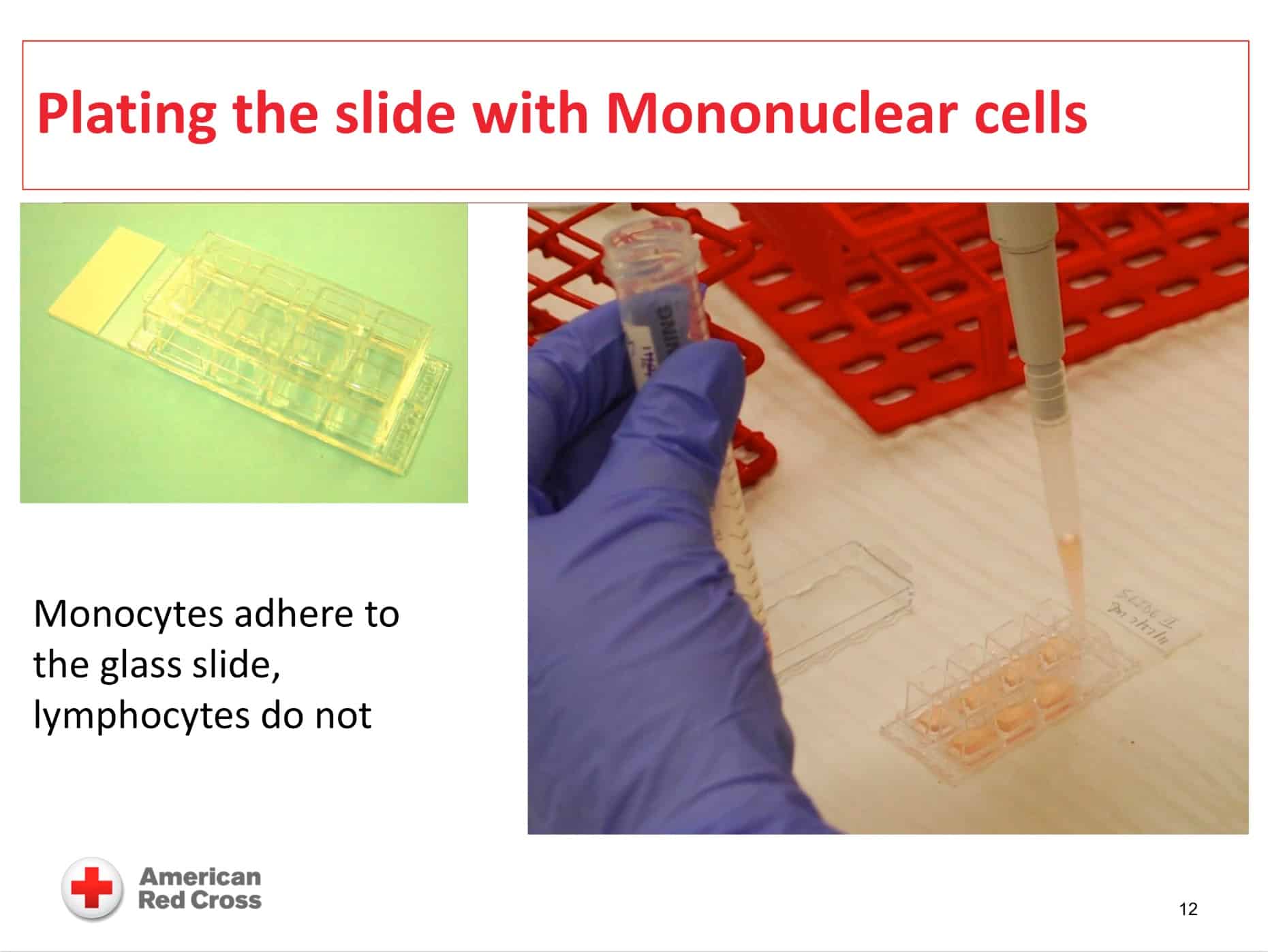
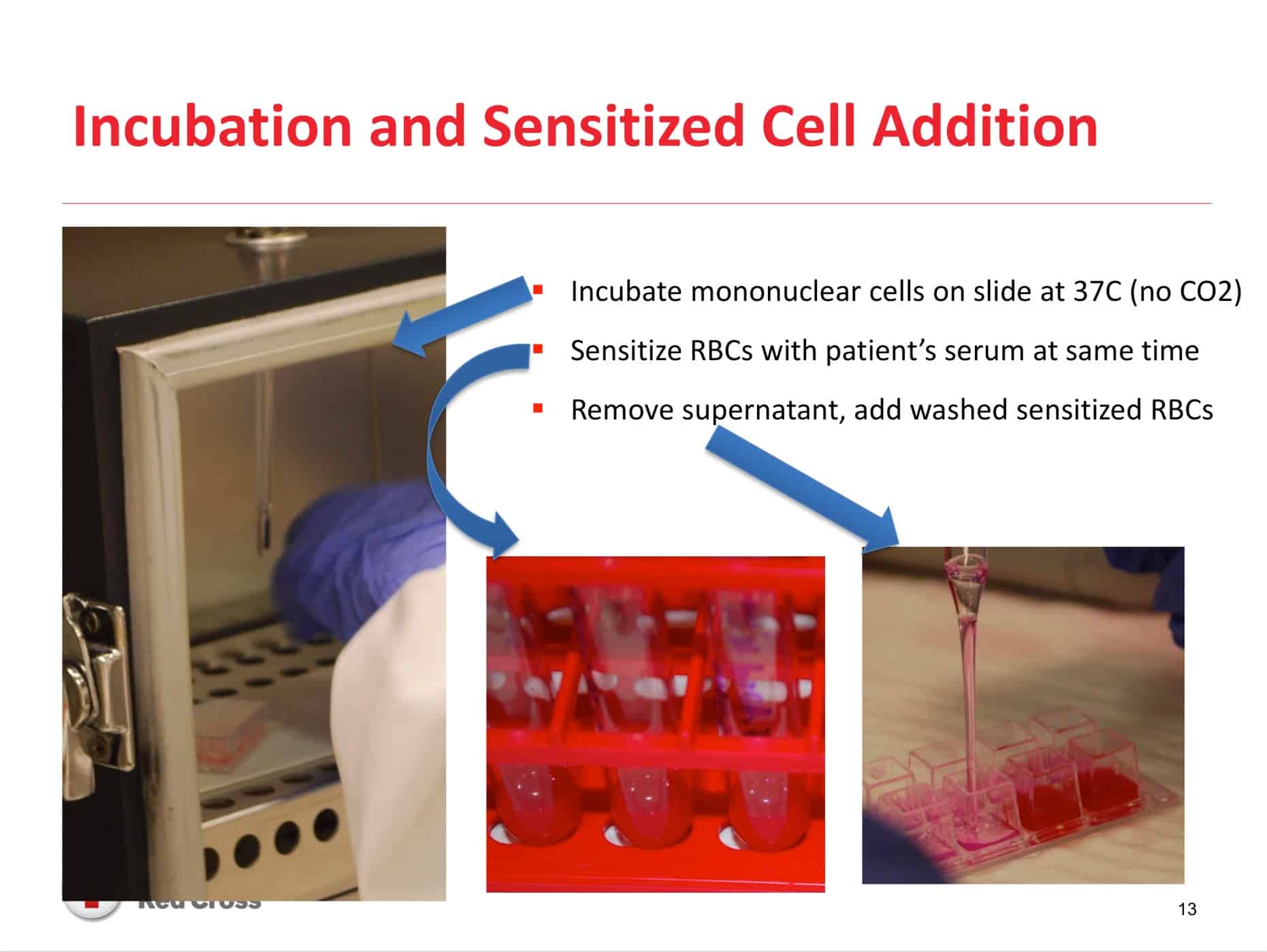
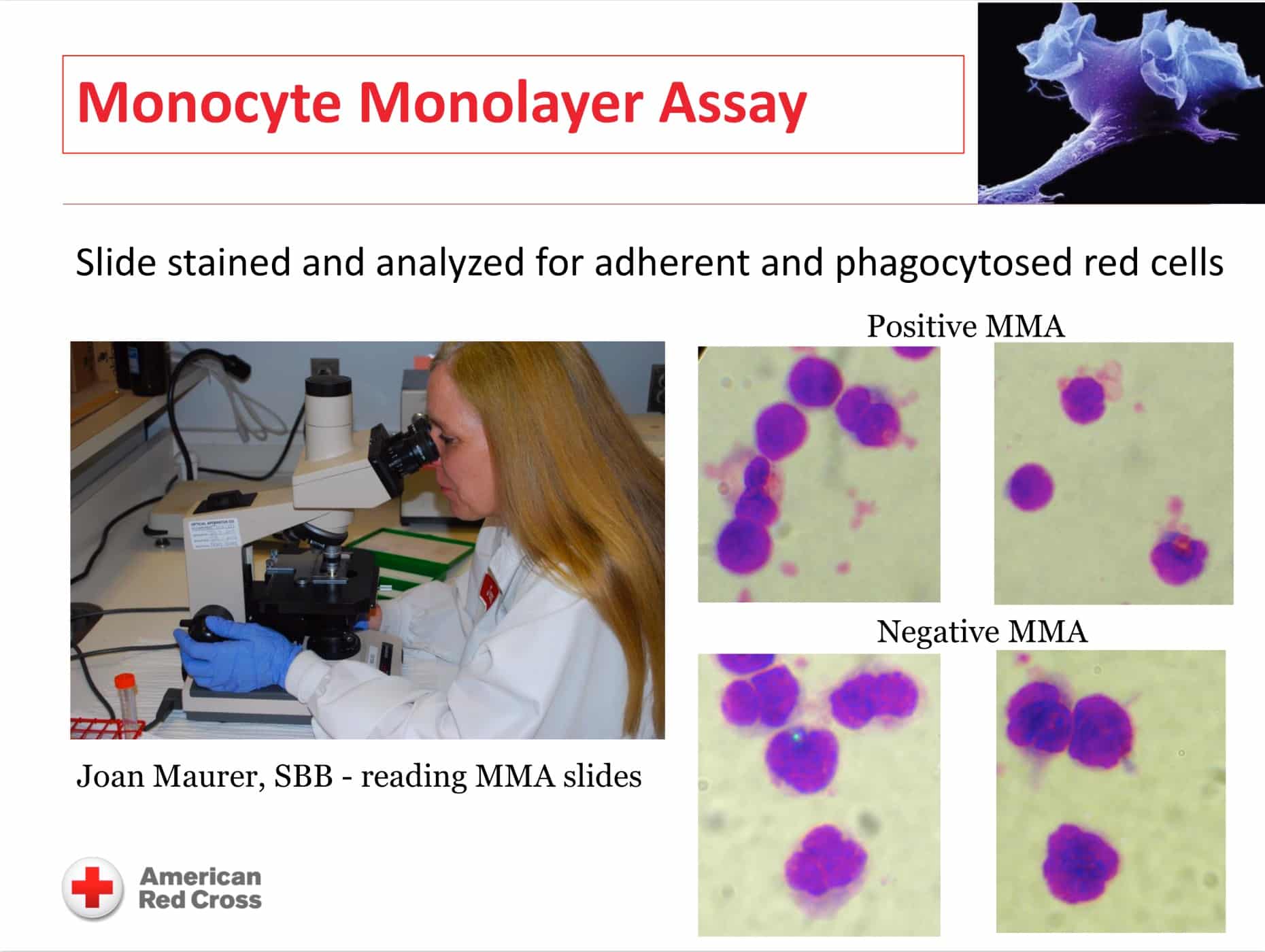
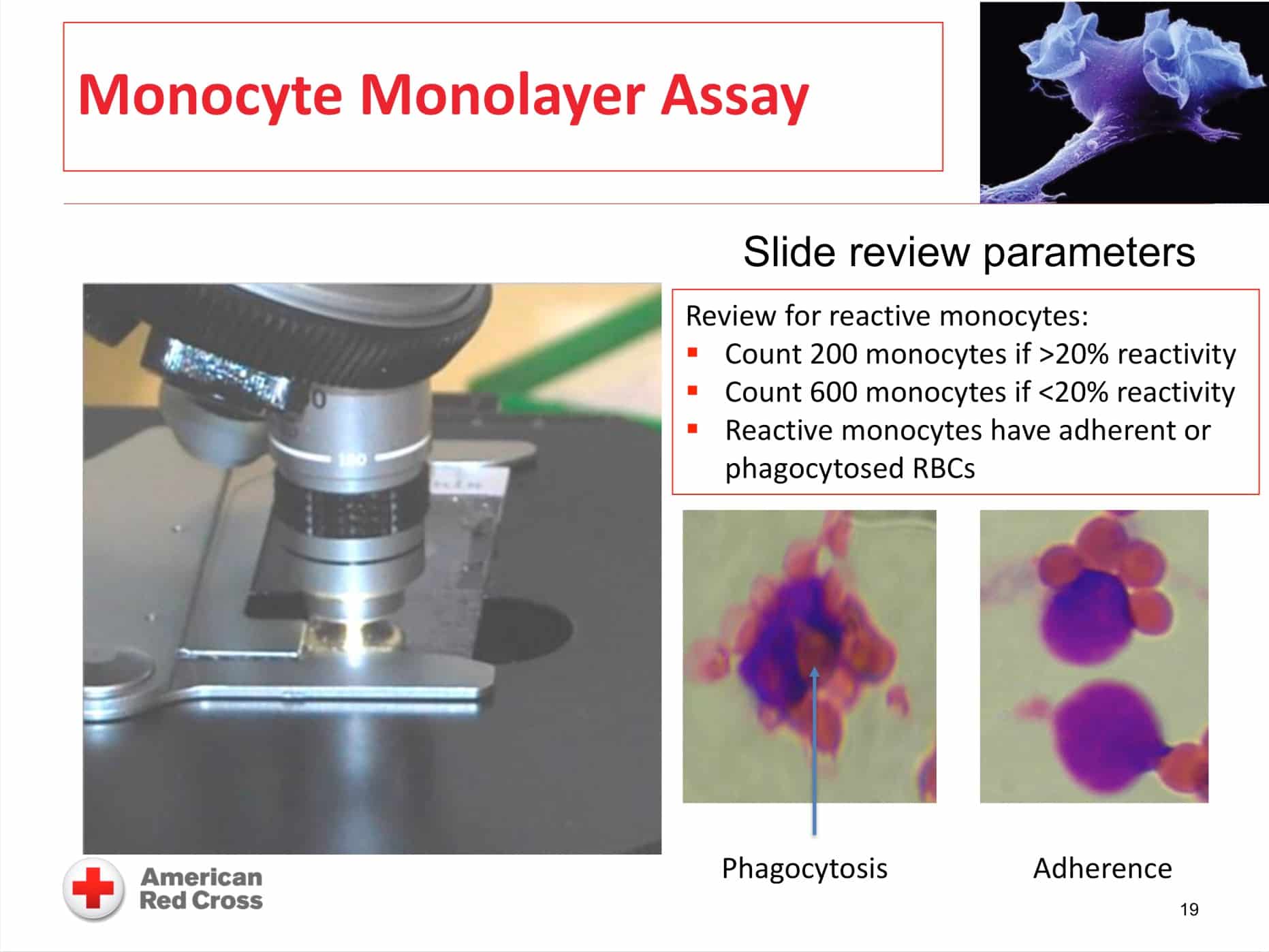
The images below are generously provided by Sandy Nance.
Further Reading:
- Original article describing the MMA: Nance SJ et al. Predicting the clinical significance of red cell alloantibodies using a monocyte monolayer assay. Transfusion 1987;27:449-452
- Retrospective review of MMA effectiveness: Arndt PA and Garratty G. A retrospective analysis of the value of the monocyte monolayer assay results for predicting the clinical significance of blood group alloantibodies. Transfusion 2004;44:1273-1281
- Maurer JL, Nance SJ, and Nickle P. Monocyte Monolayer Assay (MMA) to Predict Clinical Significance of Alloantibodies: A 22-Year Review. Transfusion 2018;58: Supplement S2:103A
Thanks to:
- Samantha Chaffin, Design and content consultant
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.